Polypharmacy in the Elderly:Causes and Solutions
1.Introduction
Polypharmacy means taking five or more medications at the same time. It’s becoming common among older adults who manage several chronic conditions.As our population ages, managing multiple chronic conditions has become common—but with it comes the heightened risk of adverse drug reactions, medication errors, and hospitalizations. This article explores the scope of the problem, its consequences, and actionable strategies for safer medication management in older adults. Learn more about personal care options for seniors in our detailed guide on Understanding Personal Care Homes and Residential Care Facilities.
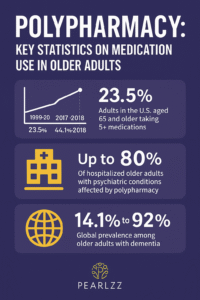
2.The Scope of the Problem
According to the National Institutes of Health, “nearly 40% of older adults take five or more prescription medications.” The CDC reports that over 66% of Americans aged 65 and older take three or more medications daily. This rise correlates with the increase in chronic illnesses such as hypertension, diabetes, arthritis, and dementia. Polypharmacy is common in older adults. However, it can cause side effects. As a result, regular medication reviews help reduce risk.
Factors contributing to polypharmacy include:
– Fragmented care across multiple providers
– Inadequate medication reconciliation
– Patient self-medication or over-the-counter use
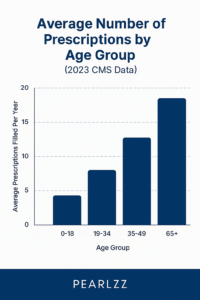
Bar graph showing average number of prescriptions by age group from 2023 CMS Data
3.Risks and Consequences
While medications are essential for managing health, their combined use can lead to serious issues. As a result of these factors, older adults face several serious medication-related risks including:
– Increased falls and fractures
– Cognitive impairment
– Drug-drug and drug-disease interactions
– Decreased adherence due to complex regimens
According to a 2020 JAMA study it found that adverse drug events accounted for 10% of hospital admissions in adults over 65—and more than half were preventable.
 Elderly lady seemingly confuse surrounded by prescription bottles
Elderly lady seemingly confuse surrounded by prescription bottles
4.Best Practices in Medication Management
Several interventions can significantly reduce the risks associated with polypharmacy:
1. Medication Reviews – Regular reviews by pharmacists or geriatricians help identify unnecessary medications and interactions.
2. Deprescribing Protocols – Involves tapering or stopping medications that may no longer be beneficial.
3. Use of Technology – Electronic health records and medication management apps improve tracking and communication.
4. Education – Empowering patients and caregivers with information about potential risks and alternatives.
‘How to Reduce Polypharmacy”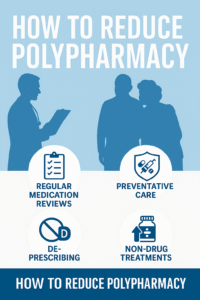
5.What Healthcare Providers Can Do
Healthcare professionals can take several proactive steps:
– Conduct medication reconciliations at every transition of care
– Involve interdisciplinary teams including pharmacists, nurses, and social workers
– Utilize screening tools like the Beers Criteria to evaluate high-risk medications
– Encourage shared decision-making with patients and families
Provider checklist graphic showing key responsibilities in medication review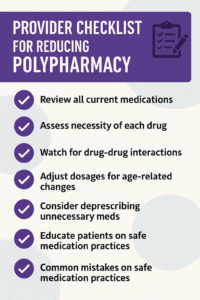
6.Call to Action: Advocating for Safe Aging
If you’re a caregiver, healthcare provider, or aging adult, it’s time to prioritize medication safety. Beyond clinical practice, addressing polypharmacy also requires broader awareness and advocacy from caregivers, patients, and communities. Begin with a conversation. Review every medication. Ask the right questions.
We can’t stop aging, but we can age smarter.
7.References (APA style)
– Maher, R. L., Hanlon, J., & Hajjar, E. R. (2014). Clinical consequences of polypharmacy in elderly. Expert Opinion on Drug Safety, 13(1), 57–65.
– Centers for Disease Control and Prevention. (2021). Prescription drug use in the past 30 days. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db427.htm
– American Geriatrics Society. (2019). Beers Criteria Update. Retrieved from https://geriatricscareonline.org/
– Steinman, M. A., & Hanlon, J. T. (2010). Managing medications in clinically complex elders: “There’s got to be a happy medium.” JAMA, 304(14), 1592–1601.